LVAD Daily Life
Sat, 11/05/2022 - 11:19AMMy daily routine:
1. Do a self-check of the controller, check the readings, and check for alarms (low flow and power).
2. Disconnect from remote power; connect to the batteries.
3. If staying-in-the house, use controller bag supplied by the hospital.
4. If going out, use fishing vest purchased from Bass Pro Shop.
5. If going out take backup bag with me. (extra controller and batteries).
6. If returning home switch to controller bag.
6. Before bed, switch out batteries with ones in backup bag.
7. Put fresh batteries in backup bag.
8. Put discharged batteries in charger.
9. To bed, disconnect from controller bag batteries to remote power.
Note: if I'm going out to get testing, I'll usually use controller bag; wires in the fishing vest will interfere with chest xrays.
Note2: I normally use wipes to clean myself; taking a shower is not easy with the shower bag and tagamart covering my driveline dressing; I have to change out the driveline dressing after shower because the tagamart sticks to the dressing.
Note3: I change my driveline dressing on Sunday morning.
Note4: Even though it is rare, I sometimes lose power, usually in the middle of the night. I had an emergency standby power generator installed ($8500.00); it cycles power within 10 secods. In 6 months this has only happened once.




Tegaderm
Mon, 11/07/2022 - 11:30AMThis will save you a lot of problems when taking a shower. I get the three fold 4x4 gauze sponges and tape it over my drive line dressing and cover it with the tegaderm. Works perfect. I take a shower every morning and my dressing never gets wet.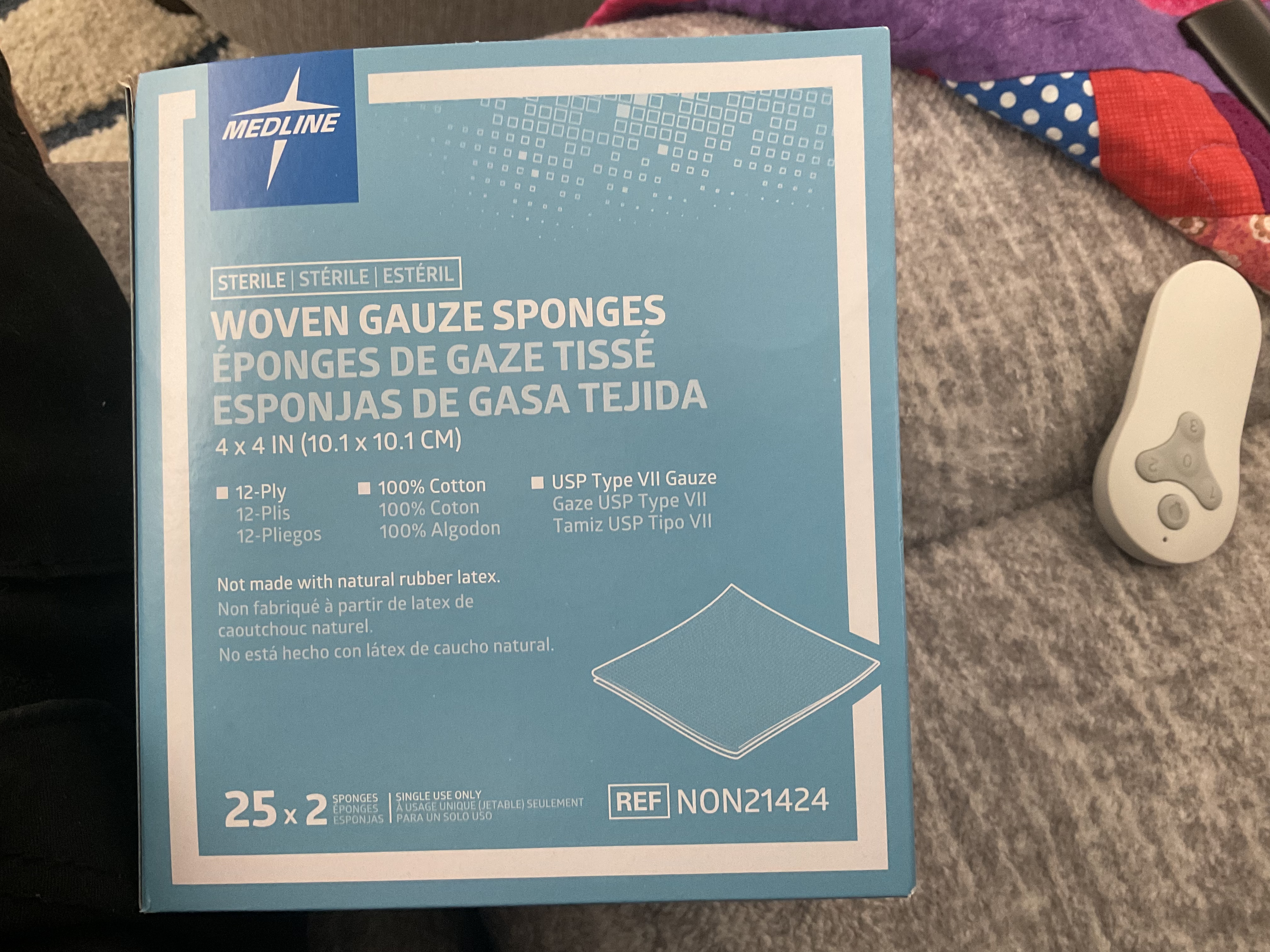
Daily Routine of an LVAD recipient
Mon, 11/07/2022 - 8:22PMGood Evening
My daily routine goes like this:
Morning
1 Wake up walk to the bathroom . a0do the normal weigh in ,wash and clean up.
2) Back to the bedroom and change the connection from the wall cord to the batteries
3 Dress in clean clothes.
4) Check the following
a) Check the Heart Mate 3 readings RPM, Flow, PI, Power, Control Battery Charge and then System Check.
b) Check and record Temp, Ox %,
have breakfast.control unit performance
Evening Wash up
Bedtime
1) Prepare the wall cord for change over
2) Select two charged batteries from the charger
3) Install the batteries as trained white first followed by the black terminals
3) Apply the Ox canular and tubing
4) Get into bed and hope I can get some sleep
Wake up and do it again.
Imm so glad I can wake uo and do it all again. Iys better than the alternative
In reply to Daily Routine of an LVAD recipient by Robert B.
MATHEW M.My Daily Routine
Mon, 11/14/2022 - 12:19PMI'm 62.
1. Wake up between 7-8am.
2. Weigh myself.
3. Drink 1 Liter of water.
4. Walk up and down stairs for about 15 minutes.
5. Workout 1hr. I do weight exercises from physical therapy. Sometimes I walk 3 miles or ride my trike 10 miles; weather permitting.
8. Do 8 minute stretch routine.
9. Take morning meds.
10. Make coffee
11. Birdbath (Shower/Dressing change every 3-4 days; more often if I sweat a lot)
12. Get dressed.
13. Eat breakfast (2 poached eggs, cauliflower, broccoli, carrots, peppers, zuchini, hot pepper cheese, avocado, meat)
14. Go to my office and work my business.
15. Take afternoon meds.
16. Lunch
17. Come home 8pm
18. Relax/Read
19. Take bedtime meds and go to sleep.
I do intermittent fasting to control my weight. I eat for 8 hours, and fast for 16 hours. I use the free version of the fastic app. 2 liter fluid minimum. 2g sodium limit.
Everyone is different.
@LVADMat on Instagram
Sponge Bath
Mon, 11/14/2022 - 11:53AMI shower once/week and use a 3M Tegaderm Film 6in x 8in over the driveline bandage. I clean up every other day using an adult wash cloth I get from Amazon. They are actually designed to clean up from incontinence but work great for a shower substitute also. I use 2-3 each time to get all areas as they are much easier than actual soap and water. I actually learned of them from a post on here! 😁
https://smile.amazon.com/gp/product/B0102FMK9G/ref=ppx_yo_dt_b_search_asin_title?ie=UTF8&psc=1
LVAD Patient
Thu, 12/01/2022 - 10:16PMHi guys, 1st time writing on here. Enjoy reading all your stories. We have a friend of my husband’s who is staying with us and he had a LVAD put in about 6 months ago. He doesn’t seem to be much better than before the LVAD. He is in bed more than out. He doesn’t really exercise unless we push him to do it. He is lazy and will admit it. I just don’t know what to think. The Dr. Said he would feel so much better after the surgery but just doesn’t seem like it. Thx for listening.
In reply to LVAD Patient by Lynn M.
ron l.Hope he begins to feel better!
Fri, 12/02/2022 - 11:39AMHi. Seems that most every post I’ve read stresses the importance of physical therapy in order to improve, which precedes doing/feeling better. Maybe not in every case, but maybe in most. All the best..
In reply to LVAD Patient by Lynn M.
Elizabeth L.My Godfather had his surgery…
Wed, 03/15/2023 - 10:31PMMy Godfather had his surgery on 1-6-23 and was on a vent all of January then they put a trach in. He hemorrhaged thru the vent 4 days afterwards since he has been on a feeding tube. Lost 45 lbs. He finally had his first meal 2 days ago. Nothing has gone the way it was promised. I don’t think his life will ever be the same . He’s 79 yrs old. He was very active before the LVAD unknown to us he had been in Afib since Oct 1st, 2022 . Was never told by Dr or company that monitors his pace maker/ defibrillator. December 19th he called me to take him to the hospital . They tell us he was in End Stage heart failure, renal & liver failure . Someone clearly messed up!
I m so disappointed in his Drs . Nothing about this LVAD has been good so far. He has had sepsis twice in CCU, blood in his urine . He can barely stand up by himself . Just very disappointing. I think they over sold this.
In reply to My Godfather had his surgery… by Elizabeth L.
Diane B.Post surgery outcome
Mon, 03/20/2023 - 7:55PMHi Elizabeth My husband went through all of that and more. He was in ICU 2 months post surgery with 2 hospital acquired pneumonias, at times swelling up and looking like the michelin man. He left the hospital on his 90 day in a wheelchair able to walk short distances only with a walker, Hickman drip for meds and a gastrostomy. Today he is totally independent in all things except dressing changes and cooks and does laundry. He has gained his muscle strength back, drives and enjoys socializing with friends and family. We were lucky to have great Home Health PT, OT and Speech to help us in the beginning. For us it was well worth having the extra years together. He is almost three years post VAD and in fact we vacationed with our family last July and celebrated our 50th there. Be strong and take one step at a time. Set achievable goals and when you reach that one reach further. Good luck !
In reply to Post surgery outcome by Diane B.
Elizabeth L.Thank you so much for your…
Tue, 03/21/2023 - 12:37PMThank you so much for your response . I appreciate it so very much . Can I ask how old is your husband ? My Godfather is 79. He’s been transferred to an Acute Rehab hospital . They finally took out the feeding tube last Wed. Starting to eat a little bit nothing taste good to him. Then this past Saturday they told me he has Candida auris. You may have read about it recently in the news . I really appreciate you responding 🙏 It gives me hope . I just get worried when he gets so short of breath just talking . 🥲
Doctors & hospitals
Fri, 03/24/2023 - 7:40PMDoes it seem like your lvad doctors are in the dark when it comes to solving some problems or answering your quesrions.
Good evening everyone I…
Fri, 04/21/2023 - 6:51PMGood evening everyone
I have had my LVAD for 4 years this may
one issue I have with my leash ( charger cord ) is it gets all twisted up and shortens it’s self up the length of 20’ is just long enough to get from one side of the house to the other side but when it’s all twisted up it shortens it’s up and when it’s twisted up it’s a tripping hazard and catches me sometimes luckily it has dropped me yet ay ideas
thank you
Hi Chuck Do you not use…
Mon, 04/24/2023 - 5:28PMHi Chuck
Do you not use your batteries during the day? I have never heard of someone staying plugged into wall unit all day long?
In reply to Hi Chuck Do you not use… by Diane B.
Lee S.Wall Unit
Wed, 04/26/2023 - 9:44AMI use my wall unit to sleep at night....that's it. Never have it on during the day
In reply to Wall Unit by Lee S.
Robert B.Wall unit
Thu, 04/27/2023 - 3:56PMI also use my wall unit only for sleeping. I make sure I control the maintenance and keeping my batteries are fully charged. I rotate my batteries for the travel kit and record it on my daily checklist for the Heart-Mate 3 to assure I maintain charged batteries for the kit.